The Art of Medicine and Stopping Smoking
 The distinguished medical journal, The Lancet, in June 2016 reported the results of a huge multinational collaborative effort to investigate the risks of psychiatric side-effects of two drugs used in smoking cessation: varenicline (Champix®) and bupropion (Zyban®); no evidence of increased harm was found compared with nicotine patches and placebo (dummy) treatments.
The distinguished medical journal, The Lancet, in June 2016 reported the results of a huge multinational collaborative effort to investigate the risks of psychiatric side-effects of two drugs used in smoking cessation: varenicline (Champix®) and bupropion (Zyban®); no evidence of increased harm was found compared with nicotine patches and placebo (dummy) treatments.
This must have been good news for the funders of this study, Pfizer and GlaxoSmithKline, who also happen to be the respective manufacturers of these drugs.
The side-effects that did occur were nausea, insomnia, abnormal dreams and headache, but, it is said, these were no more frequent in the users of these drugs compared with nicotine patches or placebo treatment.
Well, that’s nice to know. Or is it?
Were these methods any good for helping smokers quit? They found ‘Varenicline was more effective than placebo, nicotine patch, and bupropion in helping smokers achieve abstinence, whereas bupropion and nicotine patch were more effective than placebo.’ All clear?
Incidentally, the investigators only looked at smoking cessation rates at nine to twelve weeks from the start of the study. How many smokers relapsed after that we’re not told.
They recruited 8,144 smokers; and ten people contributed to the writing of the paper—all from the US except one: Professor Robert West, the self-styled world expert on smoking and addiction, who is from the UK. Of the ten authors, five were representatives of the drug companies. Of course, there was absolutely no conflict of interest whatsoever in the conduct of this study or the reporting of the results.
So, the drugs varenicline and bupropion were more helpful than placebo in getting smokers to quit and they don’t seem to cause psychiatric side-effects.
Now let me pose a question. Is stopping smoking really so difficult that you need to take a prescription drug to help you do it? But it’s worse than that: the fact that drugs are offered at all for this purposes merely reinforces smokers’ fears that quitting on their own is, indeed, difficult. Or very difficult.
A commentator in The British Medical Journal (25 June 2016, p 521) made an interesting point about this paper:
[I]t seems to me that a government serious about protecting its citizens from the harms of combustible tobacco would simply make the stuff unavailable.
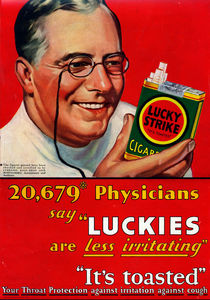
That’s the obvious solution to the smoking problem, but instead of the government taking steps, or at least talking about taking steps, to bring this about, it’s shifted the problem onto doctors. And doctors, with varying degrees of enthusiasm, have taken it up: smoking is a chronic disease; the recommended treatment includes medicinal nicotine or prescription drugs, or both. It’s almost as if smoking cessation has been hijacked by the medical profession, and in the process it’s being made more difficult.
In another post (Depression, Busy Doctors and Winnie-the-Pooh) I noted how there’s sometimes an unfortunate tendency to reduce the art of medicine to a mechanical process: diagnosis—drug. It’s operative here too: stop smoking—Zyban®.
Instead of reaching for the prescription pad, what about talking with patients? The inspirational words of a famous doctor, Sir William Osler, should be kept in mind: ‘Listen to your patient, he is telling you the diagnosis.’ And in this situation, not just the diagnosis but the key to successful treatment as well.
The doctor (or smoking cessation counsellor) needs to be interested enough to take the trouble to try and understand why smokers really smoke and why it seems so difficult for them to stop. It will then readily become apparent that all smokers are in the same situation.
They smoke because of nicotine addiction—and nothing else. The reason it seems so hard to quit is because of nicotine withdrawal symptoms. However, the withdrawal symptoms are not that bad. They consist of mental symptoms—mild anxiety and nervousness. Not uncommonly the only withdrawal symptom is a feeling or an idea of wanting another cigarette or a vague feeling of discomfort. If the smoker understands this and can be encouraged and supported not to worry about it, something wonderful will happen: it will go away!
Nicotine products and drugs are not only unnecessary but they make it harder to quit; they should not be used.
Text © Gabriel Symonds